Varicose Veins Treatment in Hyderabad
Working Time
- Mon-Thu 10:00 – 20:00
Friday 10:00 – 20:00
Saturday 10:00 – 19:00
Contact Info
-
Phone: +91 88862 41919
Ask the Experts
Varicose veins are enlarged, twisted veins that often appear dark blue or purple. They typically occur in the legs and feet, where the veins have difficulty pushing blood back to the heart. If left untreated, they can lead to discomfort and complications. Seeking Varicose Veins Treatment in Hyderabad can help relieve symptoms and prevent further issues.
Best Doctor for Varicose Veins Treatment in Hyderabad
If you’re experiencing any of these symptoms, consulting the best doctor for Varicose Veins Treatment in Hyderabad is crucial to determine the right course of action. Various treatment options, including lifestyle changes and advanced medical procedures, can help manage and treat varicose veins effectively.

What are Varicose Veins?
Varicose veins refer to veins that have become enlarged, twisted, and often swollen, typically appearing in a blue or dark purple hue. Usually located in the legs, these veins are visible just below the epidermis. They form when the valves inside the veins—which function to regulate blood flow and prevent it from moving backward—become weakened or suffer damage. This leads to blood accumulating in the veins, which in turn causes them to expand and become more noticeable. While lifestyle adjustments and conservative therapies may alleviate symptoms, some people choose varicose vein surgery to achieve greater symptom relief and enhance overall vascular health.
Who is Likely to Get Varicose Veins?
Although varicose veins can affect anyone, several factors may elevate the risk of developing this condition. These include:
Genetics: A family history of varicose veins increases susceptibility, as inherited characteristics such as weakened vein walls or malfunctioning valves can contribute to their development.
Age: Advancing age is another contributing factor, as veins tend to lose elasticity and become more prone to damage as time progresses.
Gender: Women are more commonly affected than men, with factors like pregnancy, hormonal shifts, puberty, and menopause all playing a role in vein health.
Weight and lifestyle: Excess body weight places added pressure on leg veins, and a sedentary lifestyle or lack of regular physical activity may heighten the risk of developing vein-related issues.
Occupational factors: Professions that require extended periods of standing or sitting can contribute to varicose veins, as limited movement may impair proper blood circulation and affect overall vein health.
Hormonal influences: Hormonal changes, including those experienced during pregnancy or from the use of birth control, may contribute to the formation of varicose veins.
Sun exposure : Prolonged or excessive sun exposure may damage the skin and underlying veins, and sun-related skin changes can compromise vein health.
Other medical conditions: Conditions that lead to increased abdominal pressure, such as persistent constipation or abdominal tumors, may contribute to varicose veins, and a personal history of blood clots can also impact vein function.
Causes and Risk Factors Of Varicose Veins Treatment
Varicose veins develop due to increased pressure in the veins of the legs. Common causes include:
- Genetics: A family history of varicose veins increases your risk.
- Age: Aging weakens vein valves, making it harder for blood to flow properly.
- Pregnancy: The increased blood volume and hormonal changes can cause vein problems.
- Obesity: Excess weight puts additional pressure on veins.
- Prolonged Standing or Sitting: Long periods of immobility can contribute to vein problems.
Grades of Varicose Veins
Varicose veins are categorized into different grades based on their severity:
- Grade I: Small, superficial veins that may be slightly visible but do not cause significant symptoms.
- Grade II: Larger veins that are more noticeable and may cause discomfort, including aching and heaviness.
- Grade III: prominent veins that often lead to swelling, pain, and other symptoms, requiring more focused treatment.
- Grade IV: severe varicose veins that can cause significant pain, swelling, and skin changes, such as ulcers or discoloration.

Common Symptoms of Varicose Veins
Below mentioned are several symptoms commonly associated with varicose veins:
Visible Veins: One of the most recognizable signs is the presence of enlarged, twisted, and swollen veins that are visible on the skin’s surface, often appearing dark blue or purple in color.
Pain and Discomfort: Those affected may feel pain, aching, or a throbbing sensation in the areas where varicose veins are present. After standing or sitting for extended periods of time, these sensations usually get worse.
Leg Fatigue and Heaviness: Many individuals report a persistent feeling of heaviness or fatigue in the legs, particularly noticeable as the day progresses.
Itching and Burning Sensation: The skin around varicose veins can sometimes itch or produce a burning sensation.
Night Cramps: Leg cramps, particularly during the night, may also occur in some individuals with varicose veins.
Swelling: Swelling, especially in the lower legs and ankles, can result from the buildup of fluid due to poor blood circulation.
Skin Changes: Over time, varicose veins may cause changes in the skin, including discoloration, dryness, thickening, or hardening in the affected areas.
Ulcers: In advanced cases, painful skin ulcers can form near the ankles. These sores tend to heal slowly and typically need medical treatment.
It’s worth noting that not everyone with varicose veins experiences symptoms. Some individuals may have visibly pronounced veins with little to no discomfort, while others may suffer from significant symptoms even with minimal visible signs like spider veins.
Why Recognizing Symptoms Is Important?
Early detection and timely treatment of varicose veins are crucial in preventing the condition from worsening and in relieving associated symptoms. Untreated varicose veins can result in a number of dangerous side effects, such as :
1. Superficial Thrombophlebitis : This is the term for superficial vein inflammation, which frequently coexists with blood clot formation. It can lead to localized pain, redness, and swelling in the affected area.
2. Bleeding : Varicose veins located close to the skin’s surface are more vulnerable to trauma or injury, which can result in episodes of bleeding.
3. Venous Ulcers : Sustained high pressure within varicose veins can cause skin to break down, leading to ulcers—especially around the ankle region. These ulcers may take a long time to heal and are frequently painful.
4. Deep Vein Thrombosis (DVT) : In some instances, varicose veins may be linked to DVT, a condition where blood clots develop in deeper veins. If a clot dislodges and travels to the lungs, it may cause a potentially life-threatening pulmonary embolism.
5. Chronic Venous Insufficiency (CVI) : Untreated varicose veins can contribute to chronic venous insufficiency, where the veins struggle to return blood efficiently to the heart, resulting in blood pooling in the lower limbs.
Recognizing the signs early and consulting a healthcare provider for evaluation and treatment can reduce the risk of these complications and support better long-term vein health.
Before Treatment
Before receiving treatment for varicose veins, one may experience the following symptoms:
Visible, Bulging Veins: Varicose veins typically present as enlarged, twisted veins that are clearly visible beneath the skin, most commonly in the legs.
Leg Pain or Discomfort: A common complaint includes aching, throbbing, or a heavy feeling in the legs, especially after prolonged standing.
Swelling can occur in the affected leg, particularly around the ankle and calf areas.
Itching or Skin Discoloration: Itching near the veins or noticeable changes in skin pigmentation may be observed.
Fatigue: Legs may feel unusually heavy or tired, making physical activity or even standing for long periods uncomfortable.
After Treatment
Following treatment for varicose veins, patients usually report a noticeable improvement in both appearance and comfort. Common outcomes include:
Reduced Appearance of Veins: Bulging and visible veins typically diminish or disappear entirely after procedures such as sclerotherapy or laser treatment.
Improved Comfort: Symptoms like pain, swelling, and heaviness in the legs usually subside, enhancing mobility and daily activity levels.
Smoother Skin: The skin in treated areas often becomes more even-toned and smoother as the veins fade.
Increased Confidence: Many individuals feel more self-assured wearing leg-revealing clothing such as shorts or skirts, thanks to the improved appearance.
Diagnosis of Varicose Veins Treatment in Hyderabad
Diagnosing varicose veins typically involves:
Medical History and Physical Examination: Includes inspecting the veins and discussing symptoms.
Ultrasound: A non-invasive test that uses sound waves to create images of the veins and assess blood flow.
Laser Treatment for Varicose Veins
Laser treatment is a modern and effective approach for managing varicose veins. Here’s why it might be the right choice for you:
What Is Varicose Vein Surgery?
Varicose vein surgery, also referred to as vein stripping or phlebectomy, is a medical procedure aimed at treating and relieving the symptoms of varicose veins. This treatment involves removing or sealing off damaged veins, thereby redirecting blood flow through healthier veins. It is generally recommended for individuals whose varicose veins are causing significant symptoms and have not improved with conservative measures or lifestyle adjustments. Multiple surgical techniques are available, and the choice of procedure depends on the severity of the condition and the patient’s overall health status.
Benefits of Varicose Vein Surgery
Undergoing varicose vein surgery can provide a range of benefits for individuals dealing with persistent or severe symptoms. While outcomes may vary based on the type of surgery and a patient’s health, common advantages include:

Symptom Relief : The procedure effectively alleviates pain, aching, and other discomforts by treating the root cause of the problem, leading to better blood flow and less pressure on affected veins.
Improved Circulation : By eliminating faulty veins, the surgery enhances overall blood circulation, helping prevent complications and promoting healthier vascular function.
Enhanced Aesthetic Appearance : The removal or reduction of bulging and twisted veins significantly improves the appearance of the legs, which can boost confidence and body image.
Complication Prevention : Treating varicose veins surgically reduces the risk of issues such as venous ulcers, blood clots, and skin changes, especially in advanced cases.
Increased Mobility : With less pain and swelling, patients often find it easier to move around and resume physical activities, contributing to a more active lifestyle.
Possible Complications or Side Effects of Varicose Vein Surgery
Although varicose vein surgery is generally safe and effective, it may carry certain risks and side effects. These may differ based on the surgical method employed and the individual’s medical history. Common complications include :
Pain or Discomfort : Mild to moderate pain is normal after surgery and is typically temporary. It can usually be managed with prescribed or over-the-counter pain relievers.
Bruising and Swelling : These symptoms are common around the treated area but generally improve within a few weeks following the procedure.
Infection : Though its mostly rare, at times infections can occur at the incision sites. Proper wound care and adherence to postoperative guidelines help minimize this risk.
Scarring : As with any surgical procedure involving incisions, some scarring is expected. The extent varies depending on the method used and individual healing patterns.
Numbness or Tingling : Temporary numbness or tingling may occur due to nerve irritation during surgery, though this typically resolves over time.
Blood Clots : There is a small risk of developing blood clots (such as deep vein thrombosis) after the procedure. Early mobilization post-surgery helps reduce this risk.
Allergic Reactions : In treatments involving adhesives or sclerosing solutions, minor allergic reactions may occur, though these are rare and usually manageable.
Recurrence : Despite successful treatment, varicose veins can return over time. Ongoing follow-up with a healthcare provider is essential for monitoring and addressing recurrence.
By understanding the procedure, its advantages, and potential side effects, individuals can make informed decisions and achieve better long-term outcomes with appropriate medical guidance.
Treatment Methods for Varicose Veins
The choice of treatment for varicose veins is determined by factors such as the severity of the condition, the presence and intensity of symptoms, and the patient’s overall health. The following are the several commonly used treatment options:
Conservative Treatments:
Lifestyle Modifications : Simple changes in daily habits can help alleviate varicose vein symptoms. Engaging in regular physical activity, maintaining a healthy body weight, avoiding extended periods of standing or sitting, and elevating the legs can improve blood circulation and reduce vein-related discomfort.
Compression Stockings : These specially crafted stockings exert graduated pressure on the legs, promoting better venous return, minimizing swelling, and preventing blood from accumulating in the affected veins.
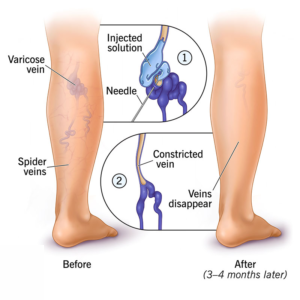
Sclerotherapy : This minimally invasive treatment involves injecting a special solution (sclerosant) directly into the varicose vein. The solution irritates the vein’s inner lining, causing it to collapse and seal shut. Over time, the body absorbs the sealed vein, improving circulation and reducing visible varicose veins.
Endovenous Laser Ablation (EVLA) : EVLA, also known as laser therapy, is a procedure that involves inserting a thin laser fiber into the affected vein. The heat from the laser causes the vein to collapse and close. Blood is then naturally rerouted to healthy veins, improving symptoms and gradually shrinking the treated vein.
Radiofrequency Ablation (RFA) : Using heat generated by radiofrequency energy, RFA targets and closes the diseased vein. Like EVLA, this minimally invasive procedure is effective and offers quicker recovery and less discomfort compared to conventional surgery.
Ambulatory Phlebectomy : This minimally invasive surgical procedure helps to remove larger surface varicose veins through small incisions. It is often recommended when veins are too large to be treated effectively with sclerotherapy or thermal ablation methods.
Laser and Intense Pulsed Light (IPL) Therapy for Spider Veins : Laser and IPL treatments are typically used for smaller veins such as spider veins. These non-invasive methods use light energy to collapse and fade superficial veins, improving the appearance of the skin.
Each of these treatments offers different benefits and may be suitable for different stages and types of vein disease. Consulting a vein specialist helps determine the most appropriate treatment plan for individual needs.
Laser and IPL Therapy for Spider Veins and Telangiectasia
For small spider veins and telangiectasia, laser therapy and intense pulsed light (IPL) therapy are often effective treatment options. These non-invasive procedures use focused light energy to heat and destroy tiny, superficial veins. As a result, the veins gradually fade away, enhancing the skin’s appearance.
Ligation and Stripping (Traditional Surgical Method)
In advanced or more severe cases of varicose veins, ligation and stripping may be recommended. Ligation involves tying off the problematic vein to stop blood flow, while stripping refers to the surgical removal of the entire vein. However, these conventional procedures are now less frequently used, as minimally invasive options like EVLA (Endovenous Laser Ablation) and RFA (Radiofrequency Ablation) have emerged, offering faster recovery times and fewer complications.
Endoscopic Vein Surgery
For complicated cases involving skin ulcers or significant vein damage, endoscopic vein surgery may be required. This procedure involves inserting a small camera (endoscope) through a tiny incision to locate and remove the affected vein with precision.
Choosing the Right Treatment
Selecting the appropriate treatment for varicose veins depends on several factors, including the size and location of the veins, severity of symptoms, the patient’s overall medical condition, and personal preferences. A thorough evaluation by a vein specialist can help determine the most suitable approach.
Laser Treatment for Varicose Veins
Laser therapy has gained popularity as an effective and minimally invasive method for treating varicose veins, especially when conservative measures such as lifestyle changes, leg elevation, and compression stockings provide limited relief.
During the procedure, laser radiation is used to seal the damaged vein. A little incision is made to introduce a thin laser fiber into the afflicted vein. As the laser emits heat, the vein collapses and seals shut. Blood flow is automatically redirected through healthy veins as the body progressively absorbs the blocked vein over time. This improves circulation, alleviates symptoms, and significantly reduces the visible appearance of varicose veins.
Faqs For Varicose Veins Treatment
Minimally Invasive : Laser therapy requires only a small incision, making it a minimally invasive procedure that minimizes scarring and reduces the risk of complications.
High Success Rate : Laser treatment has proven to be highly effective in managing varicose veins, with many patients achieving long-term relief and improved vein function.
Faster Recovery : Laser treatment provides a much shorter recovery time compared to traditional vein stripping surgery, allowing patients to return to their regular activities sooner.
Use of Local Anesthesia : The procedure is typically performed under local anesthesia, which is generally considered safer and better tolerated than general anesthesia.
Outpatient Convenience : Most laser treatments are conducted on an outpatient basis without the need of hospital stay, and minimizing overall treatment costs.
How Does Laser Treatment Work for Varicose Veins?
Laser treatment for varicose veins is a modern, minimally invasive procedure designed to effectively close off damaged veins and restore healthy blood circulation.Here’s a quick summary of what the procedure generally entails :
Assessment : Before the procedure, a thorough assessment is conducted by a vein specialist to determine the severity and location of the varicose veins. This may involve a physical examination and imaging tests like Doppler ultrasound to evaluate vein function and blood flow.
Anesthesia : To ensure comfort throughout the procedure, anesthesia is administered. Depending on the treatment plan and patient needs, this may be local anesthesia (numbing only the treatment area) or, in some cases, general anesthesia.
Laser Application :
Once the area is numbed, a small incision is made, and a thin laser fiber is inserted into the affected vein. The laser emits controlled heat, causing the vein walls to collapse and seal shut. The body gradually breaks down and absorbs the treated vein, rerouting blood flow to healthier veins.
Post-Treatment Care : After the procedure, patients are given detailed post-treatment instructions, which may include wearing compression stockings, avoiding strenuous activities, and attending follow-up appointments. In order to track healing and guarantee the best outcomes, these follow-ups are essential.
Within a few days, the majority of patients can return to their regular activities with little discomfort. For anyone looking to alleviate the symptoms and appearance of varicose veins, laser therapy provides a secure and efficient option.
Prevention of Varicose Veins
Taking preventive steps can significantly reduce the risk of developing varicose veins. Leg vein pressure can be reduced by maintaining a healthy weight. Engaging in regular exercise boosts blood circulation and supports overall vein health. It’s also important to avoid prolonged periods of standing or sitting—taking short breaks to move around can make a big difference. Additionally, elevating your legs above heart level for a few minutes daily promotes better blood flow and reduces swelling. These simple yet effective habits can help maintain healthy veins and prevent the progression of vein-related issues.
Faqs For Varicose Veins Treatment
Signs include visible, bulging veins, pain or discomfort in the legs, swelling, and a feeling of heaviness.
How does laser treatment for varicose veins compare to traditional surgery?
Laser treatment is less invasive than traditional surgery, offering reduced pain, quicker recovery, and fewer complications. Traditional methods often involve larger incisions and a longer healing process.
Yes, laser treatment is effective for many types of varicose veins, including superficial and some deep veins. Your specialist will determine the best approach based on your condition.
During the procedure, you will be comfortable due to anesthesia. Post-treatment, you might experience minimal discomfort and can usually return to normal activities quickly. Follow-up care instructions will be provided.
Laser treatment is generally safe with minimal risks. Possible side effects include mild discomfort, temporary swelling, or minor bruising. Your healthcare provider will discuss these risks and how to manage them.
Recovery time is typically short, with most patients seeing improvement within a few days and resuming normal activities relatively quickly.
Laser treatment is highly effective for many patients, especially those with severe or recurrent varicose veins. The precision of the laser allows for targeted treatment and improved outcomes.
Conclusion:
Take control of your vein health with advanced Varicose Veins Treatment in Hyderabad at Laserqure. From laser therapy to surgical options, personalized care ensures lasting relief from discomfort, swelling, and visible veins. Consult experts today for a healthier, more confident tomorrow.
